A Tennis Enthusiast’s Guide to Knee Joints: A Transcript of a Conversation with a Rehab Specialist

Beginners focus on the racket face, intermediates hone in on the core, while experts pay close attention to footwork.
As tennis technology advances, players are increasingly focusing on footwork training—yet "knee pain" remains a silent, persistent issue for most advanced players.
After experiencing a meniscus injury in my right knee, my progress in footwork training has consistently been limited by the injury—any slight increase in difficulty forces me to take mandatory rest breaks, which is incredibly frustrating.
At the beginning of the year, the author collaborated with a rehabilitation therapist to work on recovery. After some time of joint effort, "hip-knee-ankle coordination" and "bilateral knee flexibility" significantly improved, enabling effective implementation of tennis footwork training.
Here, I’ve recorded a conversation with a rehabilitation therapist about tennis-specific recovery exercises, hoping it will be helpful for tennis enthusiasts struggling with knee issues.
Record of Conversation with the Rehabilitation Therapist
Author: After injuring my knee, I’ve been feeling awkward when rotating my body during swings—specifically, "my hip joint isn’t turning fully, and I experience pain on the inside of my right knee after twisting." Could you please offer some guidance?

Rehabilitation therapist: The lower-limb coordinated movements you demonstrated primarily rely on the mobility of the "hip-knee-ankle" three joints. The main issue highlighted in the video is "limited hip-joint flexibility," which requires simultaneous strengthening of the muscles in the "ankle complex, knee complex, and glutes." The primary goal is to enhance both the flexibility and stability of each joint.
The author: "I understand what you mean by 'hip joint restriction.' In fact, I’ve intentionally been working on strengthening muscles like the gluteus maximus, medius, and minimus, as well as the piriformis, with the goal of improving hip rotation speed. But why haven’t I seen any real improvement yet?"
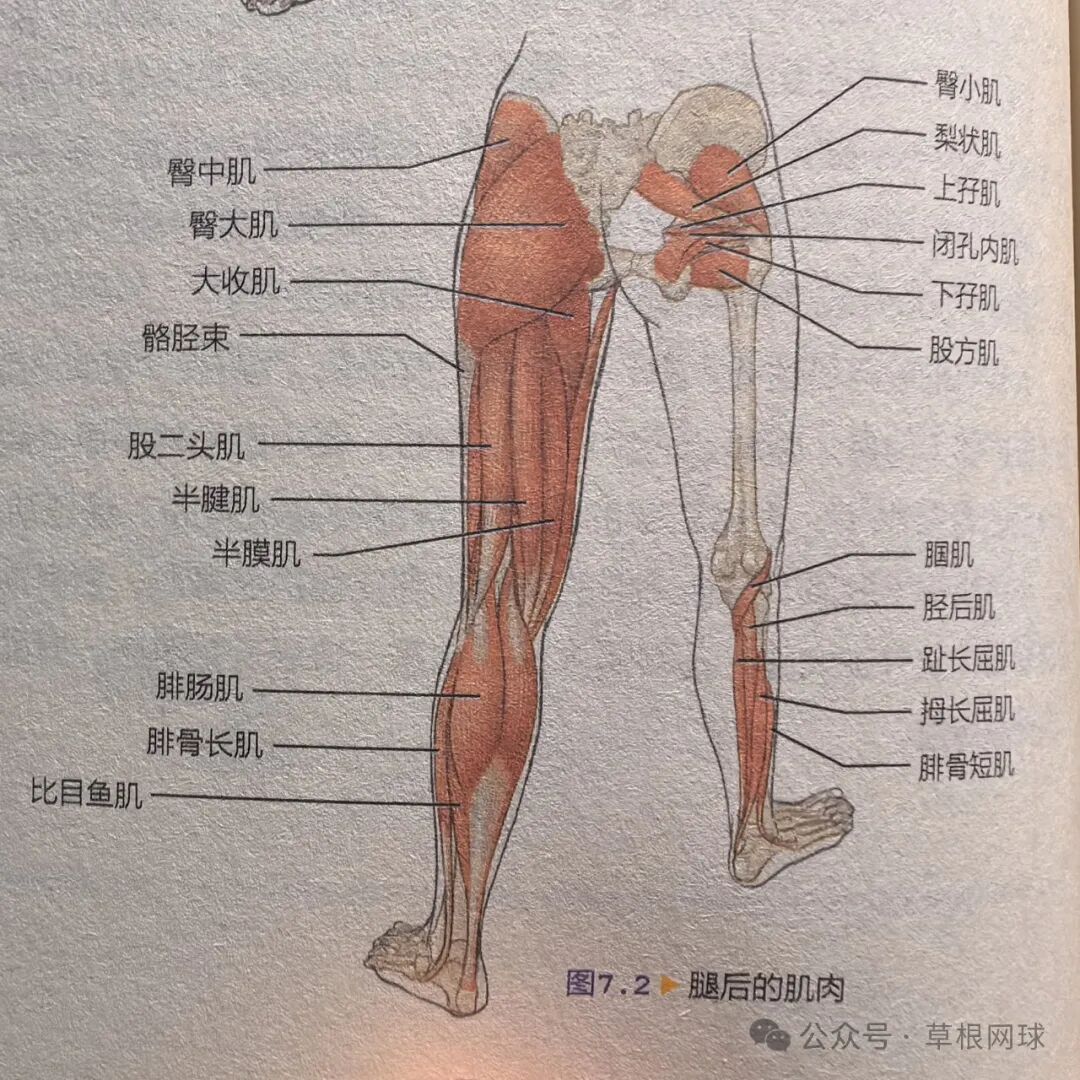
Rehabilitation therapist: The entire lower limb functions as a single unit—you can’t isolate and focus solely on strengthening the muscle groups around just one joint.
You want to increase your hip rotation speed, but right now it seems you need to focus more on building your arch and aligning your lower-limb force lines—only once this foundation is solidly established can you start strengthening further. Otherwise, your knees will only continue to worsen in pain.
Based on your postural assessment, you have a collapsed right foot arch, an off-center Achilles tendon, and hyperextension of your right knee—issues that increase the shear forces acting on your knee during movement.

Although the final result is "limited hip joint mobility," many postural issues are interconnected, with numerous indirect contributing factors.
We need to first address the underlying postural issues, and only then will strengthening your hip rotation speed naturally follow.
The author notes that some tennis coaches, when selecting players, tend to favor those with larger knee joint diameters, as these knees are better suited for high-intensity training.
Rehabilitation therapist: What exactly do you mean by "knee joint better suited for training"? I believe a good knee joint should meet at least three criteria: "space, stability, and flexibility."
First, regarding space—muscle distribution and the arrangement of bones must create room for the knee joint to move freely; otherwise, knee-joint mobility will be restricted.
Knee joint space issues need to be addressed as a priority—after all, you can’t build a dojo inside a snail shell. Athletes experiencing joint effusion or swelling caused by injury should seek medical attention promptly.
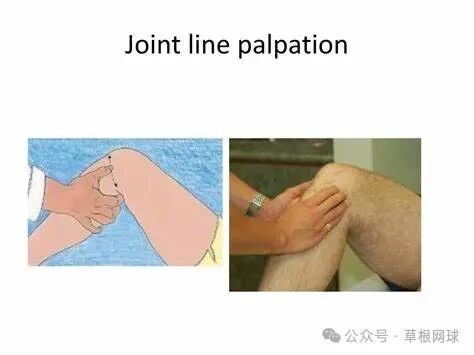
I typically use two methods—“joint space palpation” and the “patellar grind test”—to initially assess whether there are any abnormalities in the athlete’s knee joint space. Once I’ve confirmed there are no structural issues, I proceed with manual release techniques.
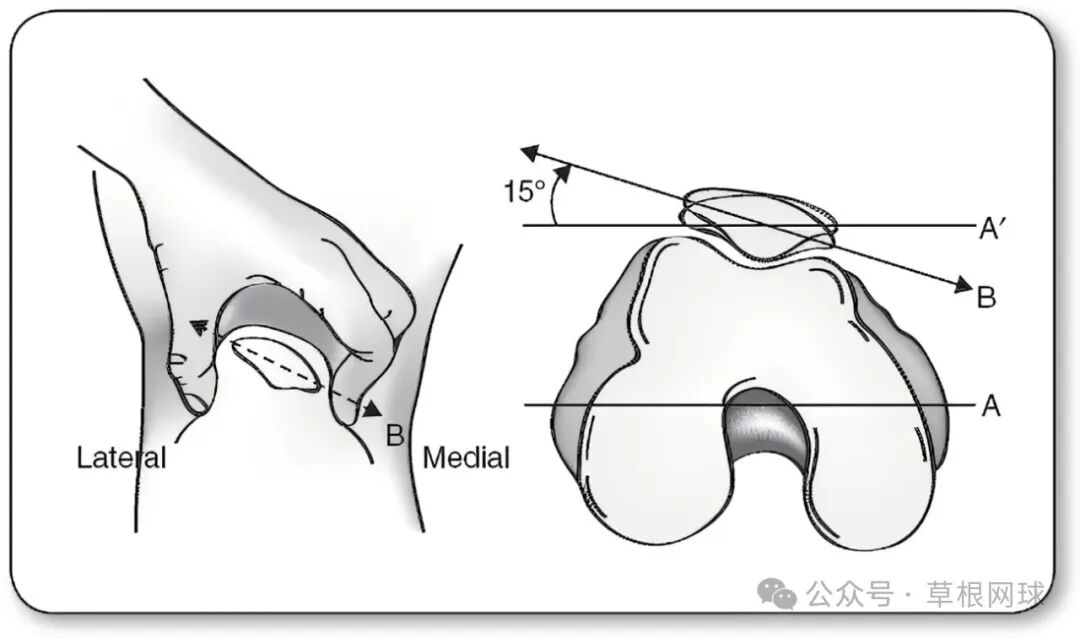
Next, let’s talk about stability: the knee joint relies on the strength and support of the surrounding muscle groups. Without this muscular support, the knee—designed originally as a hinge joint—wouldn’t be able to flex and extend smoothly along its axis, making it prone to sprains.
Let me emphasize flexibility once again: joint flexibility depends on synovial fluid, the production of which is influenced by various factors. To optimize this, it’s best to maintain a balanced diet, get plenty of restful sleep, and only engage in intense physical activity after a thorough warm-up.
Finally, it’s worth noting that the size of the joint diameter isn’t the primary factor considered by rehabilitation therapists. This is because the knee joint is naturally surrounded by muscles, and some individuals may even experience knee joint hypertrophy—meaning the joint diameter can easily fluctuate depending on various conditions. As such, relying solely on this surface-level indicator to assess joint function would be overly simplistic.
The author: I’ve now grasped the three key health indicators for the knee joint—“space, stability, and flexibility.” One final question: Some athletes take glucosamine to maintain their knees, while they rely on anti-inflammatory painkillers during periods of pain. Are there any established claims or considerations regarding these supplements and medications?
Lesong Tablets – Loxoprofen Sodium Tablets
Rehabilitation specialist: Glucosamine absorption varies from person to person. If you want to know your own metabolic and absorption capacity, you’ll need to visit a specialized institution for a thorough assessment of your body metrics. Keep in mind that results may differ depending on the individual—so if you notice positive effects, just stick with it!
Pain-relieving tablets, such as those containing loxoprofen sodium, should be taken sparingly, and topical ointments should also be used with caution, as prolonged use can lead to drug resistance.
Painkillers cannot fundamentally solve a player's knee issues—they only mask the problem temporarily. Amateur players should avoid using them blindly.
Author: Do you have any other tips for tennis enthusiasts on how to protect their knees?
Rehabilitation specialist: Knee issues should never be taken lightly—once knee pain sets in, it’s your body sending you a clear signal. Players must absolutely avoid training while injured.
At the same time, we should also adopt a holistic mindset—not just focus on addressing issues at the knees alone. The human body is an integrated system, and postural problems are closely interconnected, often creating ripple effects that influence one another.
From my experience, amateur athletes often first develop issues in their ankle joints, which frequently progress to problems in the knees. Once any of the "hip-knee-ankle" three key joints starts causing trouble, it’s crucial to schedule regular postural assessments and corrective interventions—otherwise, the situation will only worsen over time.
Life is inherently a marathon against aging—there’s no single, one-time solution for keeping your joints healthy. What we can do is make joint care a daily habit, giving it our best effort, and then pushing ourselves to go as far as only you can!


